Rehab & Training Part 2 - The Dose
Our last article and the first in this series, focused on what we called “adherence” to a training programme as a fundamental requirement of neurorehabilitation. There are some principles of strength and conditioning training that we argue can reasonably be considered to apply in the neurorehabilitation domain. The first and most fundamental principle for training success we discussed to be Adherence - after all, whether training for sport or training for neurorehabilitation, if you can’t stick to a programme you can’t expect to achieve a goal.
It is not difficult to think of barriers to adherence. For example, the cost of access to training, having to travel, results that plateau or dont meet expectations. Let’s leave these issues aside for now and assume that the initial barriers have been overcome.
We often hear that neuroplasticity and hence functional recovery, is to be exploited by using intense, task-specific and frequent, application of training. However, there is insufficient information available yet on how best to optimise these training variables for an individual case. There is also a growing recognition of the social and behavioural mechanisms (lets call it mind-set) that empower particular individuals to surprise us and recover more voluntary control of their movements than we might have expected.
In this article, we explore the second most important training principle from strength and conditioning which considers the “Dose” of training - in other words the Volume, Intensity and Frequency of training. We look at how these factors relate to neurorehabilitation and learning.
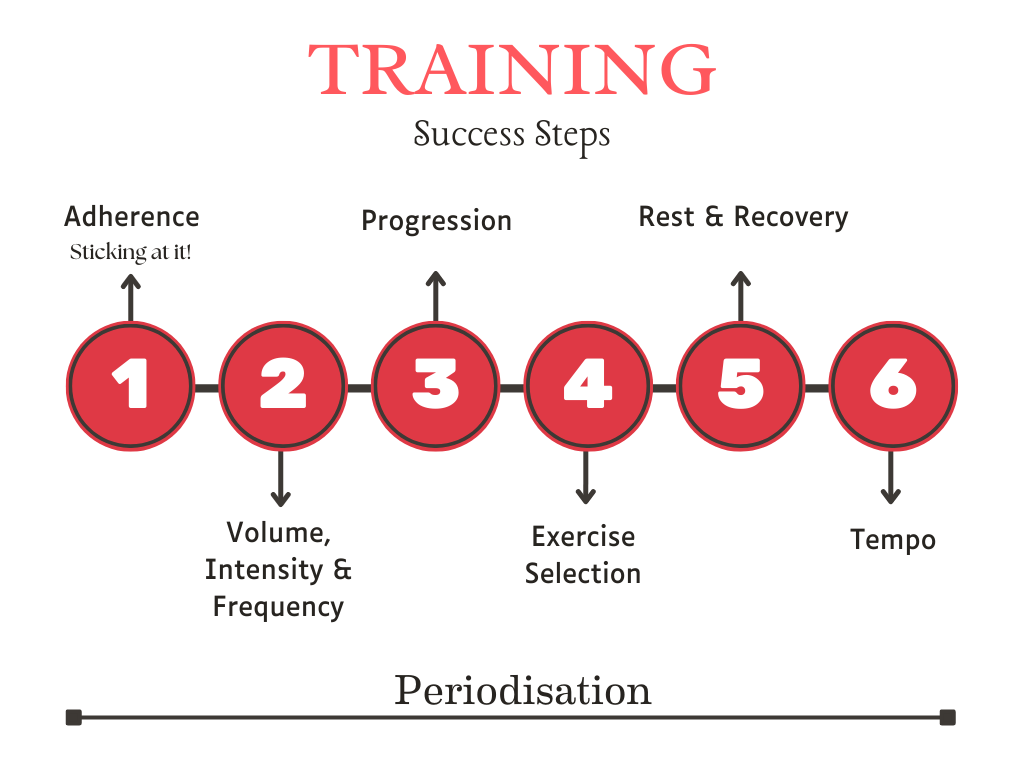
Training Success Steps
Adherence is fundamental - without commitment to a plan there is no progress. In this article we consider the second step - the Volume, Intensity and Frequency of training for the nervous system to learn
Achieving restitution versus compensation.
Enhanced recovery from a neurological insult, whether due to a stroke, traumatic brain injury or spinal cord injury, no longer appears to be an impossible dream. A growing understanding of neuroplasticity and neurogenesis has led to great optimism and progress with rehabilitation in recent years. Research suggests that we can seriously envisage restitution of function as a goal of training providing we get all the training elements correct.
However, translating the findings of clinical and animal research to routine practice is not a trivial task and we have a long way to go before we can understand the many factors involved.
The brain has a remarkable ability to grow new neurons, to reorganise cortical representations, bypass damaged neural pathways and much more. We are hungry for new therapeutic approaches that can tap into the restorative capacity of the brain and its neural networks.
We should also understand that NOT taking action at all, delaying interventions for too long, or focusing totally on compensation strategies can also produce adaption and learning in the sensory and motor cortical areas. However, this form of learning can result in “learned nonuse” - a consequence of maladaptive plasticity which is not at all desirable. In other words, the body systems capacity to adapt and learn is not always a positive thing. In “traditional” stroke rehabilitation for the upper limbs, the focus was on the importance of the first 3 months following the stroke. Passive and non-specific movement approaches were used for the affected arm and/or compensatory training of the non-paretic arm. This paradigm is not considered correct today as it results in learned nonuse.
The importance of motor learning.
It is only just over 20 years ago that studies began to appear that examined the possibility of motor learning in patient populations. At the same time, a primate model of stroke demonstrated the capability of the motor cortex to reorganise the hand representation area in response to post-injury training.
Plautz et al (2000) and colleagues went on to show that cortical reorganisation was dependent upon three commonly reported features of training. Plautz identified that cortical reorganisation was dependant on training being an intensely goal-directed, task-specific and challenging practice - this was necessary for the creation of motor learning and a result of acquiring a new motor skill.
Neuroplasticity in rehabilitation then could be thought of as learning dependent - a response to some process of applying a training stimulus and getting a beneficial outcome as a result.
Our patients don’t want to wait for another twenty years to gain progress in neurorehabilitation but much is still to be understood about how best to work. These three characteristics are open to interpretation in different ways. Lets consider these factors in a bit more detail.
Challenging practice?
There is research evidence that the difficulty of the task matters to the process of learning. The challenge is how to create a situation where practice is difficult, cognitively engaging but not impossible?
If the training is too challenging it will be frustrating and counter productive. If the training is too easy then no learning will occur.
There is substantial evidence that suggests that the difficulty of the task is very important to results. Although one can imagine manipulating a task to make it easier or more difficult, we always have the complication of individual perception. It is important that the perceived task difficulty is manipulated by the therapist by using encouragement; simple statements prior to carrying out the practice that might help improve self confidence and self-efficacy. Nothing succeeds like success.
Task-specific practice?
Specificity effects have been recognised in learning research for more than one hundred years. The general finding being that transfer of skills from repeat practice to real world application will be small unless the skills required are nearly identical in both domains.
What this means, is that general exercise and activities like strength training are most effective when combined with task-specific training programmes. Research is now looking at how practice in one task can transfer to another task in a meaningful way. This is no simple process.
For example, for the rehabilitation of motor impairments in stroke, some 19 categories of intervention have been identified from randomised trials or systematic reviews (Langhorne et al 2009, 2011)
There is no doubt that repeated attempts to solve a motor control task benefits neuroplasticity and motor learning. Available evidence seems to suggest that more is better than less training. However, tasks must not be too simple or repetitive in the sense that simple tasks well within the capability of the performer will not induce neural plasticity. What’s needed has been described as ‘repetition without repetition’.
Basically, when the body learns a new skill in movement for example, each repetition of the movement in practice will not be identical although the movement goal will be. If you imagine reaching to grasp an object a number of times, even though we manage to grasp the object each time the movement of our shoulder, arm and hand joints will not be identical in each attempt.
Skill practice must be intense?
With some of the rehabilitation programmes now being offered, promoting ‘intensity’ as important, the question arises, what is really meant by ‘intensity’? How much is this? Is it possible to overdo it?
Intensity implies that some combination of the dose - the volume, frequency and duration of training practice are important to getting results. Although this suggestion is supported by research results, there is a lack of detail when we try to pin down what exactly is a necessary and sufficient level of intensity for an individual case. We normally think of intensity in terms of a degree of concentration or an amount of applied power or force - it is not easy to visualise how to make things necessarily and sufficiently “intense.”
Some authors also point out that being able to tap into someone’s motivation to practice may actually be more effective than simply cranking up the intensity of practice. The idea here is that focusing on practice to simply reduce impairment may be less motivating than looking at seeking benefits that directly impact on the persons quality of life. The choice of task is likely to be important to results.
Volume, intensity and frequency.
Training for improvement in strength and conditioning training typically uses these three qualities of volume, intensity and frequency to describe the training variables which to some degree are interrelated.
In such training we have “rules of thumb”, increasingly backed by research, that can guide us in how to set these variables to have different effects. For example, we might describe the training volume as the number of sets and repetitions of an exercise carried out per week. Varying the intensity of effort used to carry out the volume of work is likely to produce different effects on the musculoskeletal and nervous system. Frequency relates to how often we carry out the prescribed volume of exercise.
In strength and conditioning training we know that, to a certain extent, the volume of exercise has a dose-response relationship to increased strength and/or hypertrophy (muscle size gains). However this relationship is not linear and we eventually reach the point where progress plateaus and even regresses as the volume of work increases. This is an individual characteristic and differs greatly between the novice trainee and the athlete so it is hard to generalise. There is no universal best training programme or exercise for someone to adopt.
When it comes to working with spinal cord injured persons or those recovering from neurological conditions it is equally true that there will not be one best programme to follow but the principles of exercise will surely still apply. It will be important to understand the application of adherence in each case and the variables of volume, intensity and frequency will need careful exploration. We could refer to these three variables as the exercise ‘dose’ and unfortunately we wont know beforehand how changing the dose might produce different effects.
BATRAC example - Bilateral Arm Training with Rhythmic Auditory Cueing.
As an example, we have had some experience of working with the BATRAC training approach which is based on motor learning principles and allows easy manipulation of the exercise dose. Typically It could be described as a forced-use paradigm in the form of repetitive bilateral arm training with rhythmic auditory cues. The process is task specific but does not constrain the non-paretic arm. Bilateral arm involvement in the exercise is more typical of how we use or arms in daily life.
BATRAC trainer
The patient holds the T-bars and moves the arms in time to a metronome. Movement is close to friction free. The path of movement can be changed. Counters keep track of the exercise repetitions
The video below explains the BATRAC principle in more detail.
Video explaining the BATRAC principle
In using the BATRAC trainer, patients would perhaps not be able to move the affected arm very far but would would be instructed to move both arms with the intention of keeping in time with the metronome.
They reach as far as possible with both arms to hit the counters on both sides. The exercise is demanding but novel for the patients and encourages then to achieve targets. As it is a bilateral task, it is similar in some ways to treadmill walking in gait rehabilitation, however, there is less emphasis (at least initially) on physical conditioning.
The volume, frequency and intensity of exercise were easily adjustable by the manipulation of the following variables.
duration of exercise, (5 minutes exercise followed by 5 minutes rest - repeated for up to 40 minutes at least 3 times per week)
amount of movement (gradually increasing the range of reach of the paretic arm)
rate of movement by changing the metronome beat (initially at an achievable rate and increased over time)
resistance to movement by changing the track positions (initially straight ahead, then abducted or raised incline)
phase of training (initially both arms move together and then in anti-phase - alternate arm movement)
Over time, protocols were developed to manipulate these variables in a systematic way as the patent learned the task. It is quite likely that a patient’s performance would plateau. This is as would be expected in any training programme but it was relatively easy to vary the training variables to maintain motivation and then progress.
The ASAP Model.
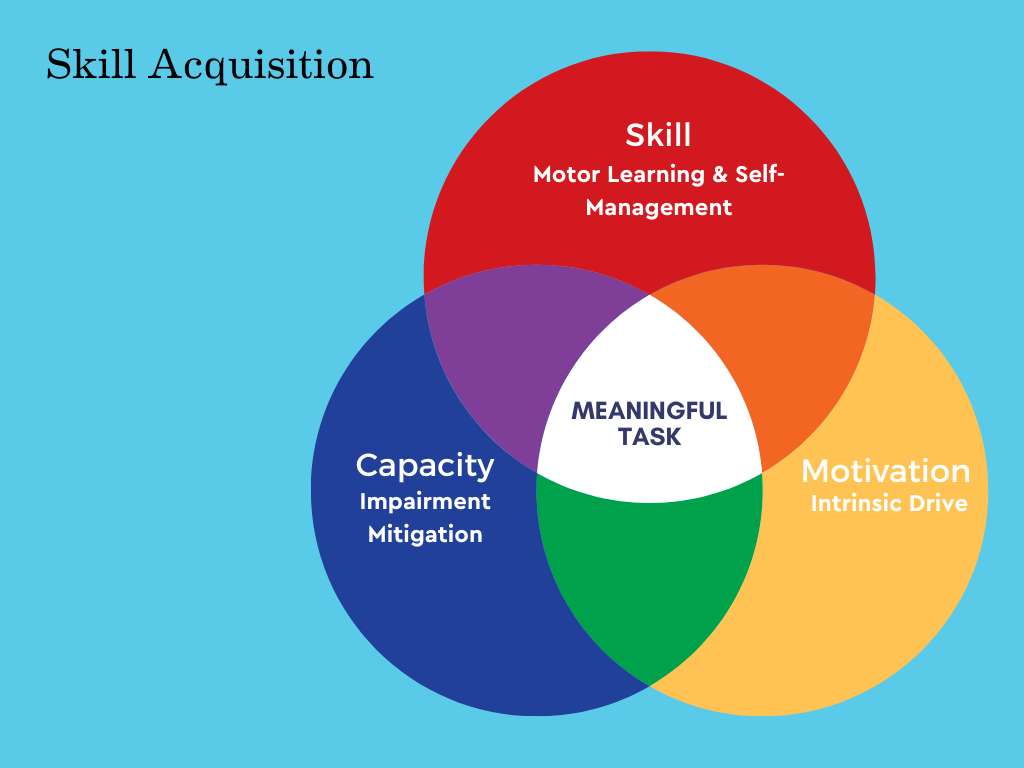
Winstein (2015) proposed what they referred to as the ASAP model (Accelerated Skill Acquisition Programme) to integrate the principles of motor learning. ASAP combines the task-specific and skill based/impairment mitigating training with patient centred motivational enhancements.
The authors suggest that skill (targeted, task-specific training) development is the most important approach to take in the case of mild to moderate stroke rehabilitation. Skill development should be focused on a task which is meaningful to the patient and supporting the reduction in impairment. As the patient makes progress, they feel more in control and confident in their own abilities.
The authors suggest that their approach, whilst drawing upon motor learning research, is influenced by exercise physiology and movement science.
Conclusion.
Exercise dose, the combination of volume, frequency and intensity, are important variables in strength and conditioning and just as important in neurorehabilitation. We are still in the early stages of understanding how to manipulate these variables to best effect with an individual. Some rehabilitation strategies such as the BATRAC principle allow easy manipulation and progression of the dose of exercise and to some extent encourage commitment to the task. The ASAP model is a useful reminder of how to blend the influence of intrinsic motivation and capacity to best effect.
In the next article we will look at the remaining training principles including exercise selection and rest and recovery.
References.
Langhorne, P et al (2009) “Motor recovery after stroke: a systematic review” Lancet Neural. 8, 741 - 754
Langhorne, P et al (2011) “Stroke rehabilitation.” Lancet 377, 1693-1702
Plautz, E.J. et al (2000) “Effects of repetitive motor training on movement representations in adult squirrel monkeys: role of use versus learning. Neurobiology. Learn. Mem. 74, 27-55
Winstein, CJ; Dorsa, BK (2015) “Translating the science into practice; shaping rehabilitation practice to enhanced recovery after brain damage” Progress in Brain Research. Volume 218, Chapter 16, 331-360, 2015