Freezing of gait: Overcoming the Challenges Faced by Individuals with Parkinson's Disease
Introduction
When it comes to Parkinson's disease, there are several symptoms that significantly impact upon the lives of those affected. One such motor symptom is freezing of gait. This gait impairment is experienced as a temporary inability to initiate or continue walking.
It can seem to arrive "out of nowhere" and last sometimes for seconds; but it can also last for several minutes. Freezing of gait can cause individuals to feel as though their feet are glued to the ground, making simple tasks like walking across a room a monumental challenge.
In this article, we delve into the complexities of freezing of gait and its profound effects on individuals with Parkinson's disease. As with many neurological conditions, the causes are not fully understood and there are a number of factors that influence the severity of freezing episodes. There is a great need for freezing of gait interventions to be personalised and adaptable to this challenging condition.
In this article we will be looking at what treatments can help with gait freezing. We introduce you to NexStride which is a clever, easy to use product, that is supported by research. NexStride brings hope to many by allowing them to self-manage these freezing episodes and regain the confidence to get their lives back on track.
Defining Freezing of Gait: Mystery Behind the Phenomenon
Freezing of gait, also known as FoG, is characterised by a sudden and unpredictable interruption in the normal rhythm of walking. In the classic presentation of fog episodes, a person feels as if their feet are stuck to the ground, making it difficult to take the next step.
What can trigger a freezing episode? These freezing episodes often occur when crossing doorways, turning around or approaching an obstacle. The severity of gait freezing is very variable from person to person, with some experiencing only occasional episodes. Rarely, some individuals will experience almost continuous gait freezing which understandably prevents useful ambulation. Often freezing of gait requires physical support from another person to get unstuck and start walking again.
While this gait disorder primarily affects individuals with Parkinson's disease, it can also be observed in those with other neurological movement disorders. Our bodies are vast networks of neural interconnections and possibilities. Just as every individual is unique, so too can be their experiences with neurological conditions such as Parkinson's.
This condition seriously disrupts lives and yet this knowledge empowers us to seek personalised care and treatment options. Support groups foster collaboration between patients, caregivers, and medical professionals. We can all navigate these challenges and continue to celebrate and participate in everyday activities, emphasising the power of human ingenuity.
Freezing of gait presents a significant obstacle to movement.
As one of the most challenging symptoms of Parkinson's disease, freezing of gait will significantly impact upon an individual's, and their wider family's quality of life. Tasks that were once done with ease, such as walking to the kitchen or getting out of a chair, become arduous and frustrating. Simple, mundane activities that most people take for granted suddenly become a daily struggle for those experiencing freezing of gait. Individuals affected can feel robbed of their quality of life and afraid to venture out from fear of being stuck or falling. If you are affected by such gait freezing episodes, then you should know that you are not alone and help is available.
Prevalence:
Viewing the Extent of Freezing of Gait in Parkinson's Disease
Research indicates that freezing of gait is a fairly common symptom among individuals with Parkinson's disease, affecting approximately 60-80% of persons at some point during the course of their illness. This staggering figure emphasises the importance of understanding freezing of gait and developing effective strategies to manage this debilitating symptom.
Freezing of gait can lead to confusion, frustration and vulnerability.
To comprehend the impact of freezing of gait, it's crucial to recognise the challenges faced by individuals with Parkinson's disease.
Imagine you are walking along a familiar path when suddenly your legs refuse to move forward, despite your brain instructing them to do so. Perhaps you are just moving from the living room to the kitchen and try as you might, you just can't seem to cross the doorway threshold. Your body feels immobilised, leaving you perplexed, frustrated, and feeling vulnerable. This is the reality for many individuals with freezing of gait. As well as this direct effect on the person with Parkinson's, it is not hard to imagine the impact on their family.
The Physical and Emotional Toll: Consequences of Freezing of Gait
Freezing of gait takes a significant physical and emotional toll on individuals with Parkinson's disease. Physically, the repeated episodes of freezing can lead to a greater risk of injuries from falls, which may result in fractures or other complications.
The very fear of falling and the unpredictability of freezing episodes can also cause individuals to consciously limit their mobility, leading to a sedentary lifestyle and further deterioration of motor function. Lack of activity rapidly leads to further weakness and increased vulnerability. This is a physical and emotional downward spiral that seems hard to arrest.
From an emotional perspective, freezing of gait can be demoralising and will erode one's confidence and independence. Tasks that were once done effortlessly now require careful planning and assistance. The inability to walk without hesitation or fear can lead to increasing social isolation, as individuals may avoid public places or events where crowds or unfamiliar environments might trigger freezing episodes. Understanding these emotional ramifications is vital in developing holistic approaches to manage freezing of gait effectively.
The Causes and Mechanisms of Freezing of Gait
Whilst the exact causes of freezing of gait in Parkinson's disease remain unclear, researchers do believe that multiple factors contribute to this phenomenon. Several factors can cause or worsen the freezing of gait, including fatigue, distraction, anxiety, stress, visual clutter, transitions from one walking surface to another, and narrow spaces. Patients who have freezing of gait also tend to experience more severe postural instability and other motor symptoms of the disease.
One possible cause involves disturbances in the brain's basal ganglia. This is a region responsible for controlling movement. These disruptions can lead to impaired communication between different areas of the brain involved in coordinating and initiating gait.
Another prominent hypothesis suggests that dopamine loss in the brain, a hallmark characteristic of Parkinson's disease, plays a significant role in freezing of gait. Dopamine is a neurotransmitter involved in various motor functions, including movement coordination. When dopamine levels diminish, the brain's ability to regulate and modulate gait initiation and execution is compromised. This disruption may contribute to the occurrence of freezing episodes.
Studies have shown that more advanced Parkinson's patients who show primarily a freezing of gait phenotype tend to have less benefit from dopaminergic medication and have more potential side effects, including motor fluctuations. Thus, there is a growing clinical focus on novel therapeutic interventions, not only for gait freezing but working on the significant non-dopaminergic pathology that exists in the primary progressive syndrome.
Patients with very severe freezing of gait episodes are often considered to be candidates for deep brain stimulation (DBS), a neurosurgical procedure which is beyond the scope of this article.
If you have Parkinson's and experience freezing of gait it makes sense to learn as much as possible about your condition. A cure of Parkinson's may not exist yet, however, effective management of gait freezing may be more likely than you think.
Decoding the Role of the Basal Ganglia in Gait Control
The basal ganglia, a complex network of structures deep within the brain, play a crucial role in the control and execution of voluntary movements, such as walking. It acts as a central hub that receives and integrates information from various regions of the brain, enabling smooth and coordinated movement.
In the context of freezing of gait, dysfunction within the basal ganglia disrupts the intricate interplay between different parts of the brain, leading to gait disturbances. Researchers have observed that abnormalities in specific areas of the basal ganglia, such as the subthalamic nucleus and the globus pallidus, are strongly associated with freezing of gait. By understanding these intricate connections, scientists can gain insights into potential therapeutic targets for freezing of gait.
The Link Between Freezing of Gait and Other Motor Symptoms
Freezing of gait often coexists with other motor symptoms commonly observed in Parkinson's disease, such as bradykinesia (slowness of movement), rigidity, and postural instability. The relationship between freezing of gait and these motor symptoms is complex, with a bidirectional influence between them.
Fear and anxiety from freezing episodes can worsen motor symptoms.
On one hand, freezing of gait can be triggered by sudden stops in movement, resulting from bradykinesia or rigidity. As walking speed decreases, the risk of freezing episodes escalates. On the other hand, the fear and anxiety stemming from freezing episodes can exacerbate motor symptoms, leading to a vicious cycle of impaired mobility.
Exploring the interplay between freezing of gait and other motor symptoms is crucial for comprehensive management and targeted interventions to address the unique challenges faced by individuals with Parkinson's disease.
Taking Action - How do you use cueing techniques to help freezing?
Article 5 & 6 listed below describes eleven approaches that have been used to combat freezing episodes. Some of these approaches involve types of training interventions and some are based on devices. Research in this area is challenging and often the best advice about any proposed intervention is first to ask "Is it safe" and then "Is it effective". In the end, this is the evidence that matters for the individual.
We are often asked should a walking stick be used? Certainly, this may help with stability and confidence. Physical therapy, especially a program that involves balance and gait training, is an essential non-pharmacological intervention to improve gait freezing and associated motor symptoms. Standardised gait questionnaires and structured physical activity programs have been used to assess patients' motor and cognitive function, providing a baseline to evaluate this and guide clinical intervention.
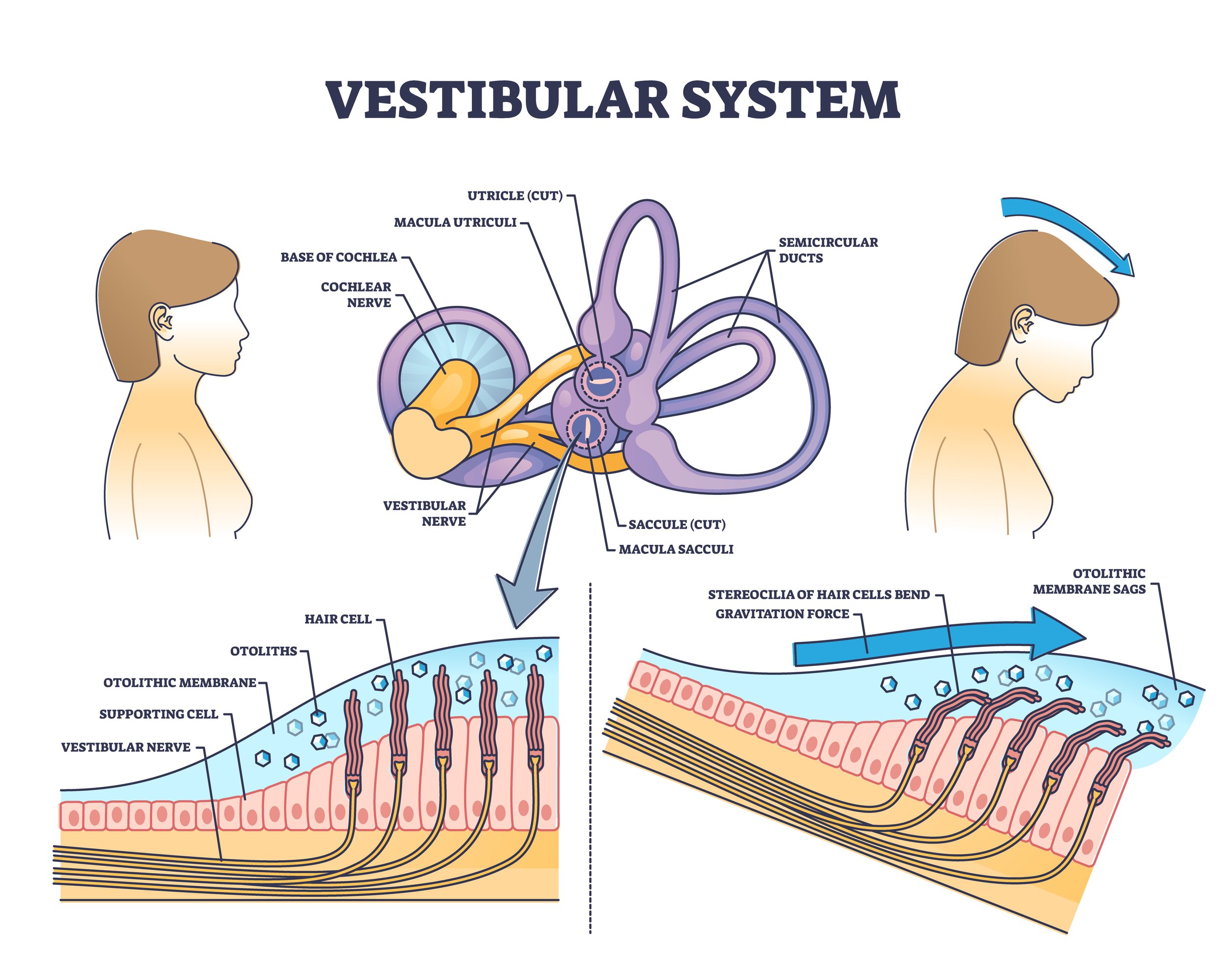
The inner ear plays a crucial role in balance and gait control; hence some research is focusing on developing novel treatment approaches that target the vestibular system. Vestibular stimulation techniques such as galvanic vestibular stimulation, can provide short-lived relief from FoG by significantly reducing the prevalence and severity of episodes.
The vestibular system is the part of the inner ear that helps control balance and movement.
Visual cues are known to be an effective method for improving freezing episodes. The presence of sensory feedback may be useful for overcoming a "motor block" and promoting movement. Various external visual cues, such as laser lines, stripes on the floor, or footstep rhythms, can be an effective way to overcome freezing, providing the patient with a predictable sequence to follow. Additionally, tasks such as mental imaging and rhythmic audio cues can also effectively trigger gait initiation in Parkinson's patients. Both visual and auditory cueing can be effective but up until now, these techniques have been lacking some refinement that could make all the difference in effectiveness.
NexStride
We hope for simply effective technology that involves very little risk to try. One such advancement is an ingenious device (the NexStride) that combines both visual and rhythmic audio cues in a novel presentation. These cues allow the individual to take advantage of new neural pathways and effectively "unfreeze" the person. Research has shown both types of cueing to be effective, but until now too little attention had been given to the human factors of convenience and flexibility.
In NexStride, these cues can be used individually or together and switched on and off as desired. Experience shows that using these cues "on demand" can often be a superior approach for many users.
This device incorporates an adjustable rhythm, similar to an electronic metronome, and a laser that projects a green line on the floor. The line serves as a visual guide, offering a predictable sequence for the individual to follow, which can be particularly beneficial in overcoming freezing episodes often experienced by those with Parkinson's.
The short video shows how the NexStride works and explains how the device can be attached to any walking cane or frame. Fundamentally by using the visual and auditory cueing, you are able to bypass the blocked neural pathway that is causing the freezing of gait.
Video explains how the device - NexStride, can be attached to any walking cane or frame.
The NexStride allows for personalisation in care, catering to the unique needs of each individual, thereby enhancing their mobility and overall quality of life.
This technology breakthrough is more than just a device; it represents hope, human ingenuity, and collaboration. It paves the way for a future where everyone, regardless of physical condition, can live life to the fullest. In the face of adversity, the human spirit shines through, as seen in the strides made in mobility for those with Parkinson's disease. Technological advancements empower individuals to reclaim independence and lead fulfilling lives. Together, we can overcome any obstacle and stride forward. Discover how NexStride can benefit you here.
Resources
Nutt JG, Bloem BR, Giladi N, Hallett M, Horak FB, Nieuwboer A. Freezing of gait: moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011 Aug;10(8):734-44. doi: 10.1016/S1474-4422(11)70143-0. PMID: 21777828; PMCID: PMC7293393.
Freezing of Gait: Comparing Treatments Options. https://www.parkinson.org/blog/science-news/freezing
Kwok, J. Y. Y., Smith, R., Chan, L. M. L., Lam, L. C. C., Fong, D. Y. T., Choi, E. P. H., . . . Bloem, B. R. (2022b). Managing freezing of gait in Parkinson's disease: a systematic review and network meta-analysis. J Neurol, 269(6), 3310-3324. doi:10.1007/s00415-022-11031-z