Combatting Pressure Ulcers: Stop the Pressure Week is here
STOP the Pressure Week during 13 to 17th November, aims to mobilise resources and prevent pressure ulcers. At Anatomical Concepts, we appreciate and applaud this initiative from The Society of Tissue Viability. The Society is collaborating with The National Wound Care Strategy Programme (NWCSP) and all four UK nations, to emphasise that when it comes to pressure ulcers, 'Every Contact Counts'. There is a recognition that the first step to pressure ulcer prevention is generating the widest possible awareness in the community of how to recognise those at risk and take steps for prevention. In this article, we review some of the main themes that relate to the topic of pressure ulcer prevention. We also describe our particular interest in heel pressure ulcer prevention and treatment with the PRAFO range of devices.
What are pressure ulcers?
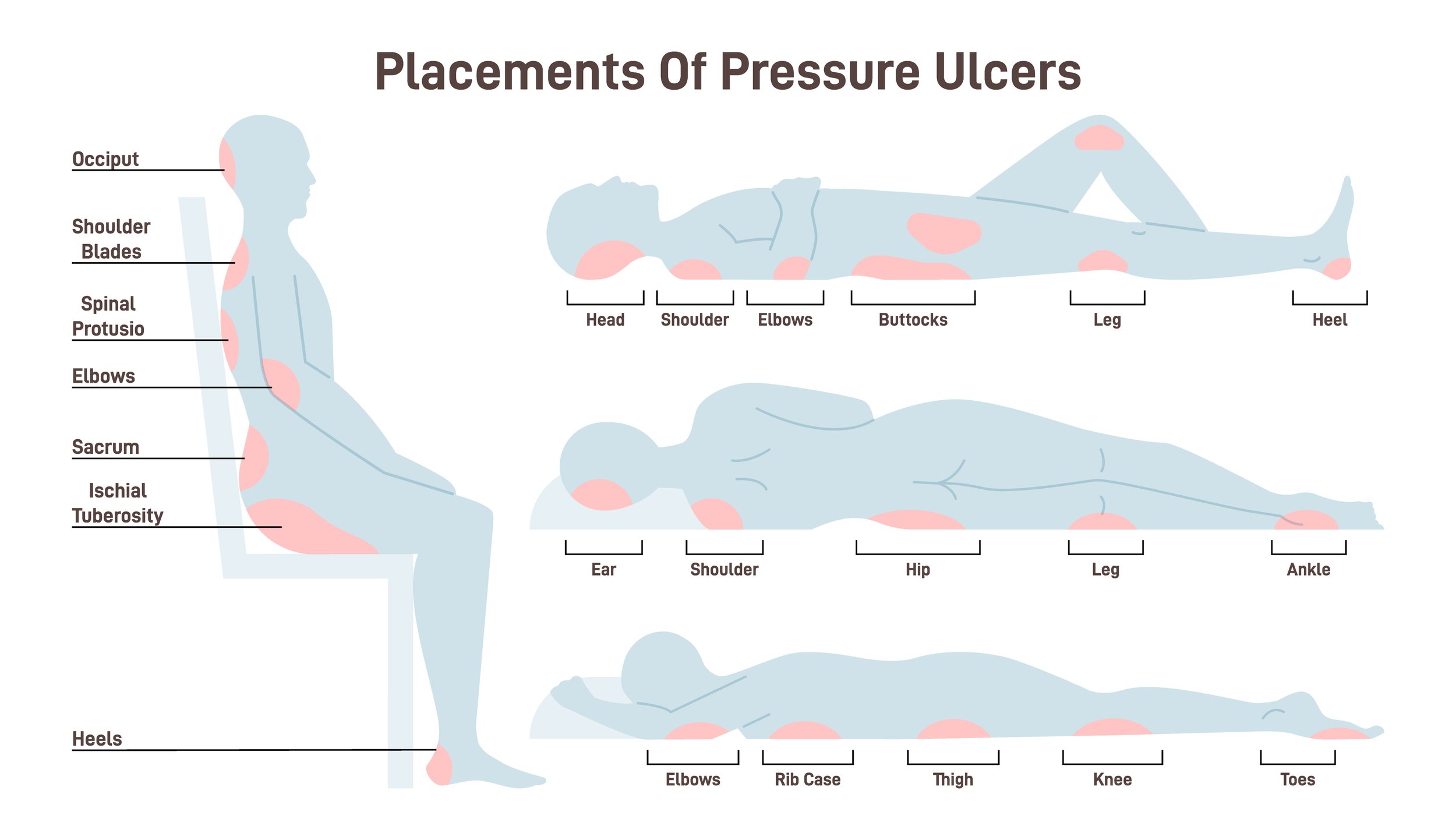
Pressure ulcers, in the past, known as bedsores or pressure sores are localised injuries to the skin and underlying deeper tissue. These usually develop over bony areas of the body in contact with a support surface such as a bed or wheelchair. They form due to prolonged periods of pressure, or pressure in combination with shear or friction. Areas that are frequently susceptible to pressure ulcers include the back, shoulders, elbows and sacrum, hips and heels; especially in vulnerable individuals confined to bed or a chair for extended periods. The risk of pressure sores is influenced by what we could call "mechanical factors" as well as medical ones. We will explain what influences risk in more detail below.
These pressure ulcers are best prevented as they can lead to severe medical complications. Even when ulcers do heal, the tissue in that area will be at greater risk of breakdown in future due to changes in the structure of the tissue which becomes less elastic.
Prevention starts with recognising the risk
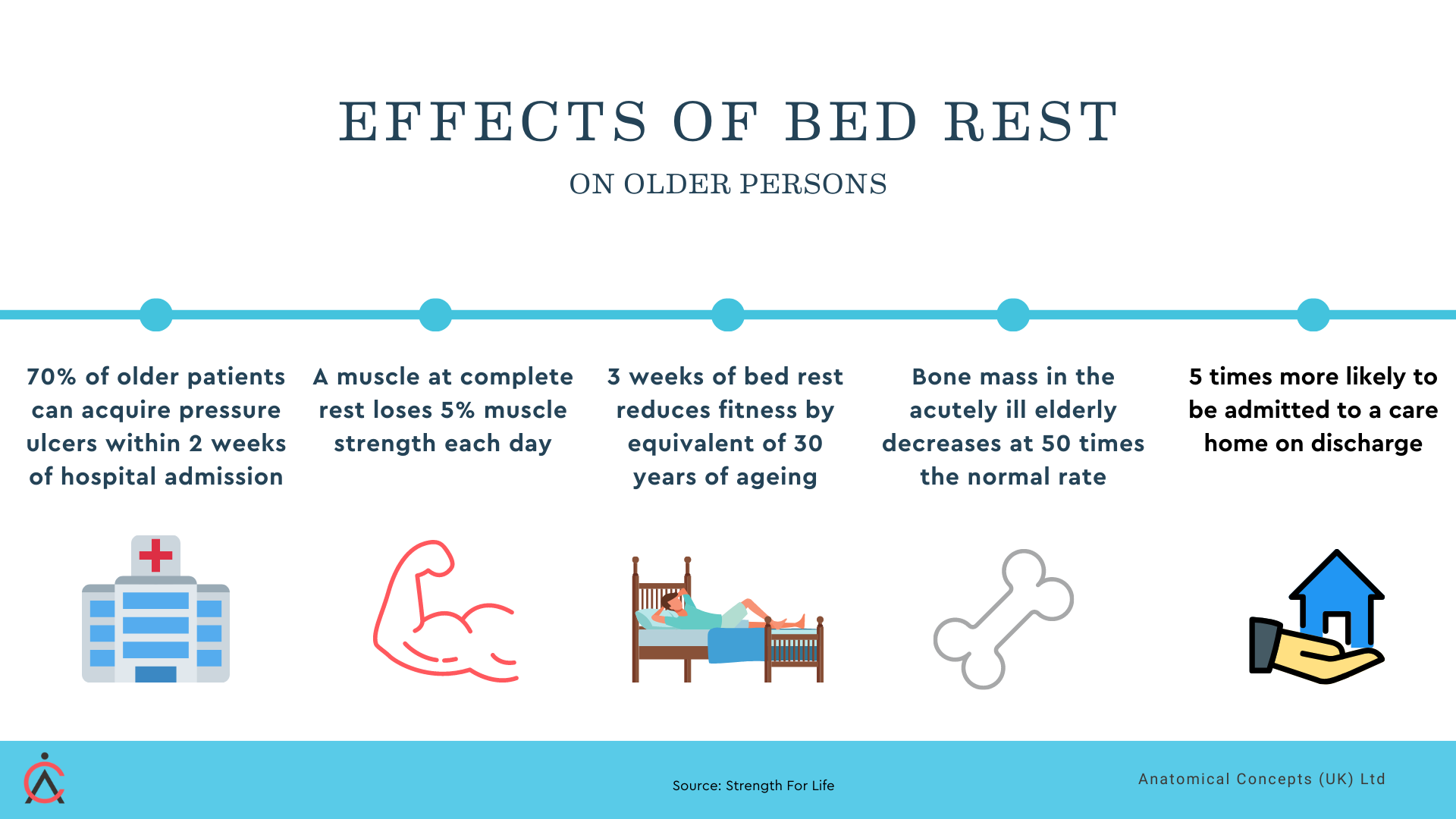
For many years, medical science has understood that pressure ulcers are often preventable but despite this, they are still often seen in hospitals, care homes and the community. The financial and human cost of acquired pressure sores is high. To some extent, an ageing and unfit population is likely to mean that many more persons are going to be at risk of pressure ulcers.
The effects of bed rest - increased vulnerability to pressure ulcers
For all of my career of more than fifty years, I have seen what I thought was broad recognition of the risk of pressure ulcers and yet they still are frequently seen in clinical practice. When working in North America, I saw that pressure ulcers were considered a "failure of care". It is certainly true that in many cases they can be prevented but this is not always easy. We have to recognise too that the person who develops a pressure ulcer is often dealing with some primary medical condition and the ulcer is a side effect.
As I mentioned above, pressure ulcer risk is influenced by both medical and mechanical factors. I have described these in earlier articles on our website but will briefly outline the main points here.
Medical risk factors are many and have been described many times in the medical literature as they lead to increased susceptibility. These factors include:
sensory impairment - perhaps due to spinal cord injury or other neurological condition; neuropathy with diabetes
level of consciousness
Incontinence or skin moisture, which can weaken the skin's integrity and lead to skin breakdown
tissue mass - bariatric or obese patients
reduced mobility
extremes of age - sarcopenia
malnutrition and dehydration
previous ulceration changes to the structure of the affected tissue making future breakdown more likely
ASCVD - vascular diseases that compromise circulation and tissue health
Mechanical risk factors include pressure, shear and friction between vulnerable points of the body and the support surfaces in place. It is important to note that pressure ulcers are not some tissue surface effect; they involve deeper tissue structures and indicate that the mechanical effects of pressure and shear are not just felt at the skin surface. We need to be alert to poor manual handling techniques - for example moving a person on a support surface can result in elevated friction and shear between the heel and the support surface.
Prevention necessarily involves recognising and managing both mechanical and medical risk factors. Treatment too must pay attention to both factors. Medication and wound dressings might be necessary but are often not sufficient to ensure successful treatment.
A podiatrist colleague put this very well when it came to treating diabetic foot ulcers. He would say, "It is not what you put on an ulcer that heals it (lotions and potions) but what you take off (pressure and shear)
Good skincare helps prevent heel ulcers.
Preventing heel ulcers is key to avoiding the pain and discomfort associated with these wounds. Simple steps to prevent heel ulcers include regular repositioning, reducing pressure on bony areas by using pressure relief devices (ideally the PRAFO see below), good skincare, and managing medical conditions that can contribute to ulcer development. Regular foot checks can also help identify early signs of infection or skin breakdown that can lead to ulcers. Early intervention is crucial for preventing complications associated with pressure ulcers, such as infection, tissue loss, or nerve damage. If a patient does develop a pressure ulcer, healthcare professionals should provide prompt intervention to promote wound healing, prevent infection, and manage pain. This may involve referral to a wound care specialist or other healthcare professional with expertise in pressure ulcer management and wound care.
Our concern with heel pressure ulcers
Before choosing a heel protector, it’s important to understand the different types available. Some commonly available types include simple foam, gel, air-filled, and sheepskin-lined "bootee" structures.
Foam and gel protectors are typically relatively inexpensive and provide moderate pressure reduction, whilst air-filled protectors offer more customisation and adjustability. Sheepskin-lined protectors are soft and comfortable, but may not provide as much pressure reduction as other types.
At Anatomical Concepts, we have a very successful product that has proved itself a valuable tool for the prevention and treatment of heel ulcers. The original PRAFO (Pressure Relief Ankle Foot Orthosis) was developed about 30 years ago as a result of seeing many elderly persons develop heel pressure ulcers whilst on bed rest following hip fractures. The aim was to create an orthosis that was easy to apply, would provide total pressure relief to the vulnerable heel area and also provide protection once the patient was able to be mobilised.
The 652SKG features an adjustable metal upright, intrinsic walking base, and various liner options
The PRAFO proved successful because of this combination of features. Foam pads, strategically placed cushions and other similar products might seem to be adequate for pressure sore prevention but these only reduce the pressure, whereas the PRAFO designs totally suspend the heels and provide absolute pressure relief.
Further than this, the PRAFO designs encouraged continuity of care because they would provide protection against the development of contractures at the foot and ankle and provide heel and ankle protection when it became time to mobilise the patient. All the PRAFO designs such as the 650SKG, 652SKG or 653SKG feature metal upright structures, an intrinsic walking base and a range of liner options.
A simple "Heel Protector" may be sufficient to protect the heel with some patients but these will never prevent the development of contractures or allow the patient to be protected whilst ambulant. It comes down to choosing a product based on a careful assessment of risk and of the clinical objectives now and in the future.
From the pressure ulcer point of view, why do we think zero pressure at the vulnerable area is better than reduced pressure?
Pressure ulcers arise when the combination of applied pressure or shear and time exceeds a critical threshold. The problem is we don't know where that threshold is and it varies significantly from person to person. Each person's medical risk is a compounding variable.
Consider two situations that could result in a pressure ulcer when a person's heel is in contact with a support surface.
1) the pressure applied at the heel is low but is present for a long period
2) the pressure applied at the heel is high but is present only briefly
The threshold for the development of ulceration is influenced strongly by a person's medical risk factors, age and the nature of the support surface in contact with the heel. This being the case, the only way to eliminate the risk of pressure ulcers is to use a device that eliminates the pressure such as the PRAFO design. Low pressure is not good enough.
In all cases, we need to think of what are the medical and mechanical risk factors in this specific case.
Conclusion
In conclusion, the prevention and treatment of pressure ulcers is a multifaceted issue that relies on addressing both medical and mechanical risk factors. The PRAFO designs by Anatomical Concepts stand out as effective tools in managing these risks, providing total pressure relief to the vulnerable heel area and encouraging continuity of care by protecting against contractures, and enabling mobilisation. These designs consider each individual's unique medical risk factors, thereby offering a tailored approach to ulcer prevention. However, it's crucial to remember that while products like PRAFO designs are beneficial, a thorough assessment of risk factors and clinical objectives should always be the base of any prevention or treatment strategy.
Additional reading