The Impact of Spinal Cord Injury on the Human Body
Spinal cord injuries have profound and lasting effects, disrupting both physical and neurological functions. Understanding these consequences is vital for patients, healthcare professionals, and researchers working towards improving outcomes for those affected. This brief guide will explore the physical challenges caused by spinal cord injuries, supported by insights from medical experts and research while highlighting potential treatments and solutions.
When the spinal cord is damaged, communication between the brain and body is disrupted. Depending on the severity and location of the injury, this disruption can result in paralysis, loss of sensation, or other debilitating symptoms. By comprehending these impacts, we can better develop treatments, therapies, and assistive technologies that improve quality of life.
Read on to gain a detailed understanding of how spinal cord injuries affect mobility, muscle control, and sensory functions—and the advances aiming to overcome these challenges.
Causes of Spinal Cord Injury
Spinal cord injuries (SCIs) arise from diverse causes, generally grouped into traumatic and non-traumatic origins:
Traumatic Causes
Traumatic injuries occur due to accidents or sudden impacts that damage the spinal cord and surrounding vertebrae. Examples include:
Motor vehicle accidents
Falls
Sports injuries
Violent acts (e.g., gunshot or knife wounds)
These incidents often lead to fractures or dislocations that compress the spinal cord. Prevention efforts, such as road safety education and protective equipment, are key to reducing these injuries.
Non-Traumatic Causes
Non-traumatic SCIs result from underlying conditions that deteriorate spinal cord function over time. Causes include:
Tumours
Infections (e.g., bacterial or viral)
Medical conditions like multiple sclerosis (MS) or amyotrophic lateral sclerosis (ALS)
These injuries tend to develop gradually, making early detection critical. Diagnosing and addressing these conditions promptly can minimise damage and improve treatment outcomes.
Socio-Economic and Lifestyle Factors
Certain factors increase the risk of SCIs, including high-risk occupations, extreme sports, and inadequate access to healthcare services. For instance, individuals lacking timely medical care may experience delayed diagnoses, worsening their prognosis. Addressing these lifestyle factors and socio-economic inequalities can play a key role in reducing SCIs. As our population ages we are seeing more injuries due to falls.
Types of Spinal Cord Injury
SCIs are categorised based on their severity and the resulting impact on bodily functions. The injury is classified by what is called an ASIA score but in simple terms the types of injury might often be described as so-called "complete: or "incomplete".
Complete vs. Incomplete Injuries
Complete injuries: Total loss of sensory and motor function below the injury site, indicative of severe spinal cord damage.
Incomplete injuries: Partial preservation of sensory or motor function, allowing varying levels of movement or sensation. These injuries offer greater potential for recovery with targeted rehabilitation. However, we should say that even with complete injuries, it is rare for the spinal cord to be severed entirely. Even those with complete injuries may be able to recover some function.
Location of the Injury
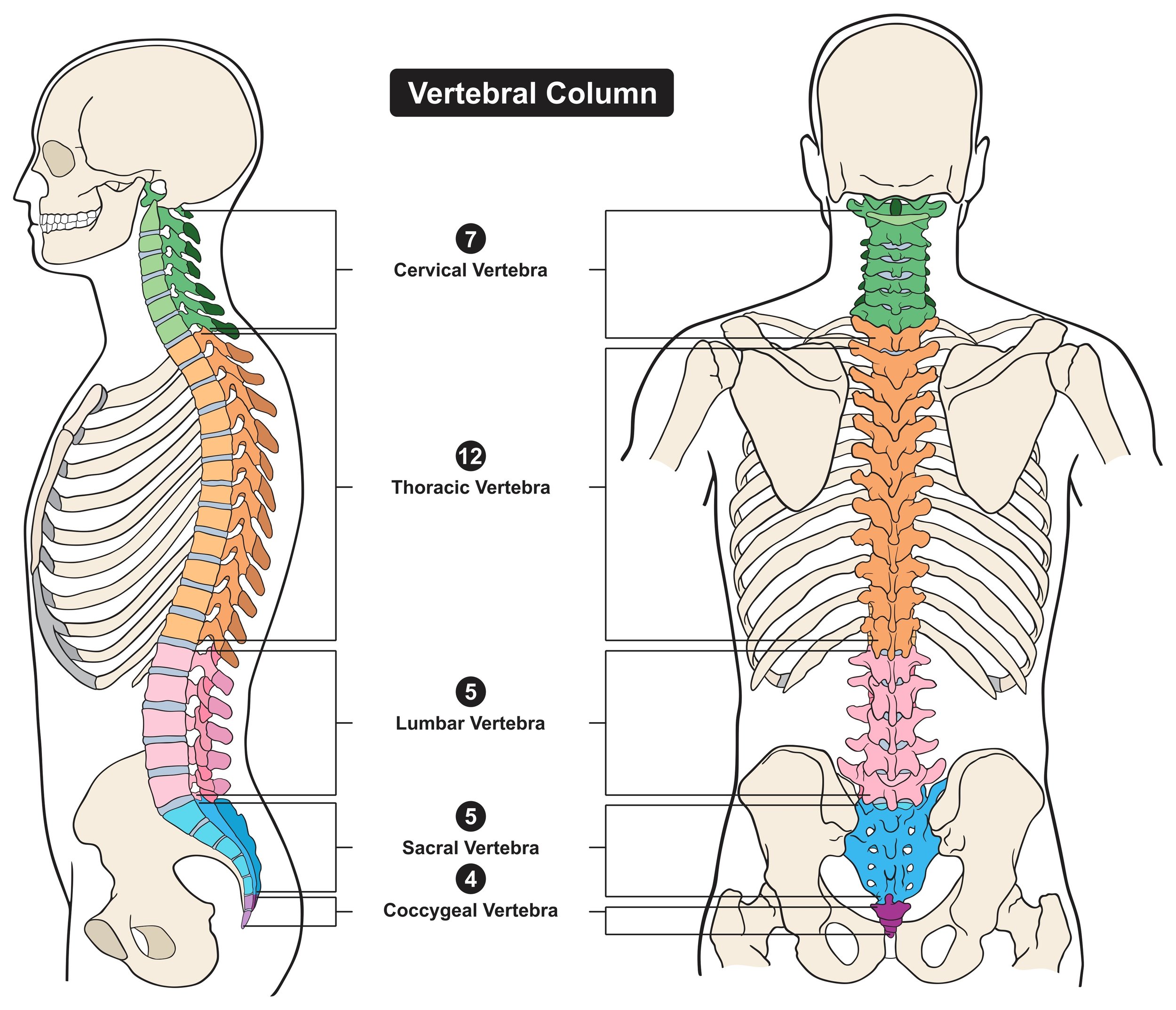
The location determines the affected bodily functions:
Cervical (neck): Injuries result in tetraplegia, affecting all four limbs.
Thoracic (upper back): Typically cause paraplegia, impairing lower limbs but sparing upper body movement.
Lumbar/Sacral (lower back): May impact lower body and bladder/bowel function.
Mechanism of Injury
SCIs can also be classified by how the damage occurred—flexion, extension, rotation, or compression injuries. Each mechanism impacts symptoms in unique ways, aiding diagnosis and treatment planning.
Immediate Effects of Spinal Cord Injury
The initial aftermath of a spinal cord injury is often severe and life-altering. Understanding these effects is critical for early intervention.
Physical Symptoms
Paralysis: Sudden loss of movement, often dictated by the injury’s location on the spinal cord.
Loss of Sensation: Numbness or the inability to feel pain, touch, or temperature below the injury site.
Autonomic Dysfunction: Disruptions in essential functions like blood pressure, heart rate, and temperature regulation require urgent attention.
Psychological Impact
The emotional shock following SCIs can be overwhelming. Patients often experience feelings of fear, confusion, and uncertainty about their future. Early psychological support is crucial to help manage anxiety and adapt to their new reality.
Medical Complications
Acute-phase symptoms like spasticity and autonomic dysregulation demand prompt medical intervention to stabilise the patient and prevent further harm.
Long-Term Physical Consequences of Spinal Cord Injury
Over time, spinal cord injuries give rise to significant physical and systemic changes:
Mobility and Muscle Function
Loss of Mobility: Permanent paralysis may require wheelchairs or assistive devices. Mobility limitations impact independence and necessitate major lifestyle adjustments.
Muscle Tone Changes: Increased spasticity (stiff muscles) or flaccidity (weak muscles or denervated muscles) can lead to complications like joint contractures and pressure sores. Continued physical therapy helps mitigate these risks.
Systemic Effects
Respiratory System: Weak diaphragm muscles in high-level SCIs increase vulnerability to respiratory conditions like pneumonia.
Cardiovascular System: Issues such as orthostatic hypotension (sudden drops in blood pressure) are common, requiring ongoing monitoring.
Gastrointestinal System: Reduced bowel function impacts digestion, necessitating dietary changes and specialised care.
Adopting a holistic approach that addresses all affected systems is essential for effective long-term management.
Secondary Complications Associated with Spinal Cord Injury
Secondary complications often arise from SCIs, significantly affecting quality of life:
Pressure Ulcers: Prolonged immobility increases the risk of skin breakdown. Preventative measures include frequent repositioning and pressure-relief devices.
Urinary Tract Infections (UTIs): Catheter use often leads to recurrent infections. Adopting proper bladder management protocols helps minimise risks.
Mental Health Challenges: Feelings of isolation, depression, and anxiety are common. Access to counselling and support groups promotes emotional resilience.
Proactively managing these complications is vital for improving long-term outcomes for those with SCIs.
Moving Towards Hope: Advancing SCI Treatments
Research and innovation are at the forefront of improving lives affected by SCIs. Today, rehabilitation therapies, cutting-edge assistive devices, and experimental treatments—such as stem cell therapy—promise to restore lost function and independence.
Understanding the physical consequences of spinal cord injuries not only highlights the challenges experienced by patients but also underscores the importance of healthcare, education, and innovation in this field.
By fostering greater awareness and supporting advancements in neurorehabilitation, we can build a future where individuals with spinal cord injuries achieve their highest potential.
Rehabilitation and Management of Spinal Cord Injury
Rehabilitation plays a pivotal role in the recovery journey for individuals with spinal cord injuries, focusing on maximizing independence and improving quality of life. The rehabilitation process often begins in the acute care setting and continues through outpatient services. A multidisciplinary team, including physiatrists, physical therapists, occupational therapists, and psychologists, collaborates to establish personalized goals and treatment plans. This team approach ensures that all aspects of the patient's health and recovery are addressed.
Physical therapy is a cornerstone of rehabilitation, helping to improve strength, flexibility, and mobility. Therapists utilise various techniques to enhance physical function, including therapeutic exercises, gait training, and assistive technology. For individuals with incomplete injuries, early mobilisation and rehabilitation can lead to significant improvements in motor and sensory function. The goal is not only to restore physical abilities but also to empower individuals to regain control over their lives.
In an ideal world, rehabilitation aims to restore as much function as possible and compensate for what cannot be recovered. This way we tend to see technology for persons with SCI aimed at restoration or compensation.
Occupational therapy complements physical rehabilitation by focusing on enhancing daily living skills and promoting independence. Therapists work with individuals to develop strategies for performing tasks, such as dressing, cooking, and personal hygiene, adapted to their abilities. Additionally, vocational rehabilitation services can assist individuals in returning to work or pursuing new career opportunities, fostering a sense of purpose and fulfillment. This comprehensive approach to rehabilitation is crucial for achieving the best possible outcomes for individuals with spinal cord injuries.
Assistive Devices and Technology for Individuals with Spinal Cord Injuries
Innovations in assistive devices and technology have revolutionised the lives of individuals with spinal cord injuries, offering solutions that enhance mobility, independence, and overall quality of life. Among these, wheelchairs remain indispensable, serving as vital tools for navigating daily environments. Modern powered wheelchairs, equipped with advanced features like joystick controls and adaptive seating, offer unparalleled autonomy and ease of use. These advancements not only improve physical mobility but also empower individuals to actively engage in their communities and social activities. Equipment such as FES bikes and FES technology can restore or preserve the muscle tissue and bring benefits to circulation and overall health. Preventing long term complications is important. All of us need to exercise, eat well and look after our mental and physical wellbeing.
Beyond wheelchairs, a new wave of assistive technologies is reshaping possibilities for those with spinal cord injuries. Exoskeletons, for instance, are wearable robotic devices that enable individuals with lower limb paralysis to stand and move. The Tek RMD for example combines an ability for a paralysed person to stand with the ability to move around.
The Tek RMD assists a user with paralysed legs to both stand and move around in their environment
These groundbreaking tools provide more than just physical mobility—they also boost psychological well-being by restoring confidence and a sense of normalcy. As technology progresses, the potential for new innovations to aid rehabilitation and daily living will continue to grow.
Communication technologies are another essential aspect of assistive tools. For those with limited mobility or fine motor control, voice-activated devices, adaptive keyboards, and eye-tracking systems offer vital support. These technologies enable seamless communication, access to information, and computer use, helping to combat isolation and foster mental well-being. The integration of such tools into rehabilitation strategies demonstrates the transformative potential of technology in enhancing daily life for individuals with spinal cord injuries.
The Psychological and Emotional Impacts of Spinal Cord Injuries
The psychological and emotional repercussions of spinal cord injuries are profound, yet often overlooked. The abrupt loss of physical ability can trigger a range of emotional responses, including shock, grief, anger, and depression. Many individuals find it difficult to adjust to their new reality, struggling with feelings of loss and longing for their pre-injury lifestyle. Without proper support, these emotional challenges can hinder rehabilitation and diminish overall quality of life.
Mental health support plays a critical role in helping individuals navigate the emotional complexities of spinal cord injuries. Therapy and counseling provide safe spaces to process emotions and develop healthy coping mechanisms. Support groups, where individuals share experiences and encourage one another, foster a sense of belonging and resilience. These connections can mitigate feelings of isolation, offering both comfort and empowerment.
The emotional impact of a spinal cord injury extends beyond the individual to their family members and caregivers. Loved ones often face their own challenges, such as adjusting to caregiving roles, managing feelings of helplessness, or worrying about the future. Providing education and emotional support for families is essential, equipping them to better cope with their own struggles while supporting the individual with the injury. Addressing these psychological dimensions is crucial for comprehensive care and recovery.
Conclusion: Thriving with a Spinal Cord Injury
Living with a spinal cord injury brings unique challenges but also opportunities for growth, adaptation, and resilience. While the physical effects can be life-altering, the right combination of resources—rehabilitation, assistive technologies, and mental health support—can help individuals regain independence and improve their quality of life.
Building a supportive community is equally vital. A network of healthcare providers, family, and friends can offer encouragement, practical assistance, and understanding. Raising awareness about spinal cord injuries further drives research, innovation, and improved treatment options, paving the way for better outcomes for those affected.
Ultimately, life with a spinal cord injury is not defined solely by limitations but by the strength, determination, and adaptability of those who face it. By embracing support, leveraging advancements in technology, and fostering resilience, individuals can live fulfilling, dignified lives. As we move forward, let us work toward a future where people with spinal cord injuries can thrive with autonomy, hope, and the unwavering support of their communities.