Pressure ulcers: The common risk factors
Pressure ulcers are a significant problem in the UK, particularly for bedridden patients or those with limited mobility. They occur in up to 23% of patients in acute care facilities and up to 33% of patients in long-term care facilities. At Anatomical Concepts, we are particularly interested in heel pressure ulcers, accounting for approximately 25% of all ulcers.
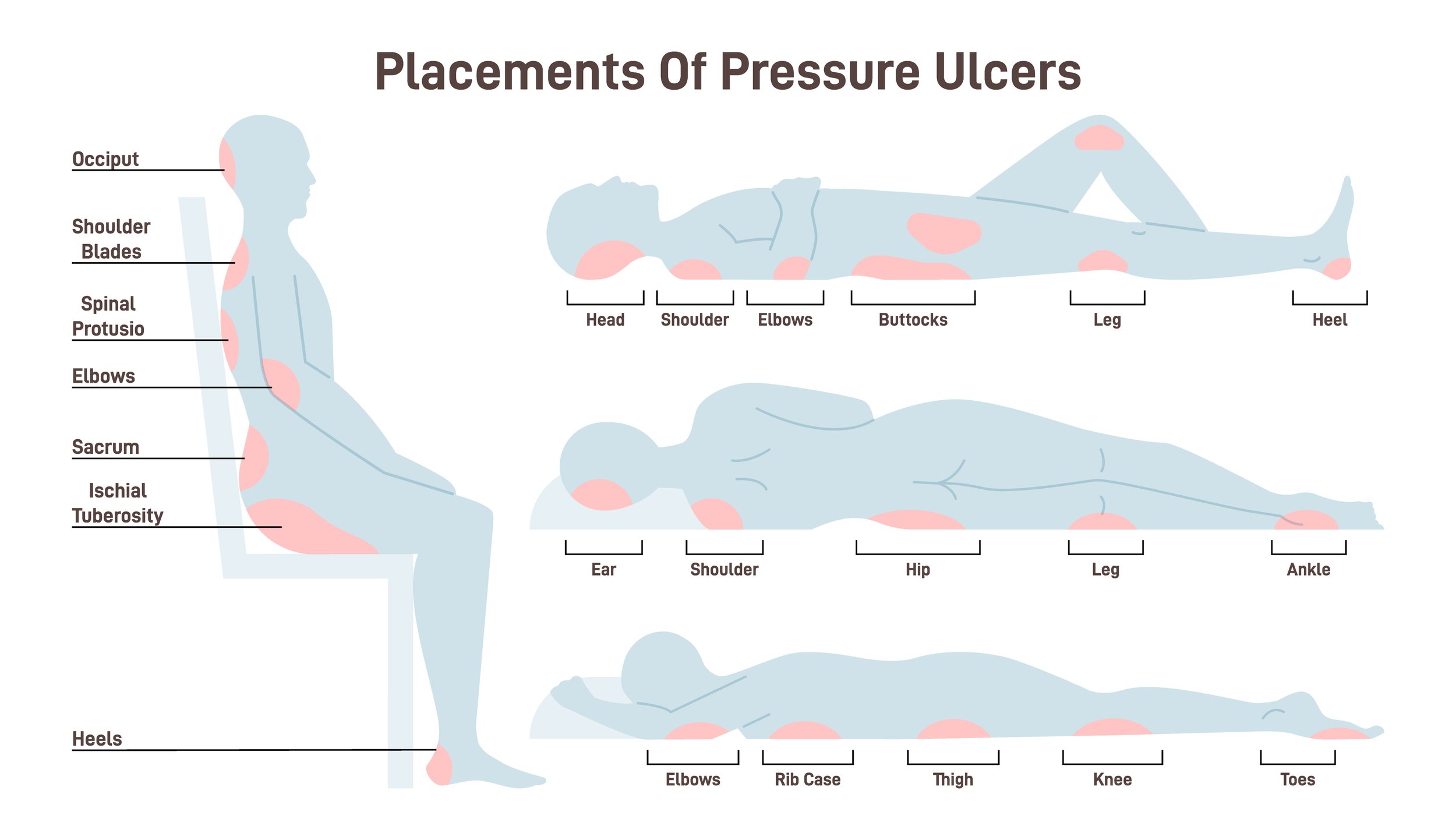
Pressure ulcers typically occur over bony prominences
Regarding the economic impact, heel pressure ulcers can result in increased healthcare costs due to prolonged hospital stays, additional treatments, and the use of specialised equipment such as pressure-relieving mattresses and aids, wound dressings, and medication. A study published in the Journal of Wound Care estimated the annual cost of pressure ulcers in the UK to be between £1.4 billion and £2.1 billion, with heel ulcers accounting for a significant portion of this cost.
Additionally, heel pressure ulcers can significantly impact patients’ quality of life, causing pain, discomfort, and a decreased ability to perform daily activities. They can also lead to complications such as infections and sepsis, which can further increase healthcare costs and mortality rates.
Therefore, preventing and effectively managing heel pressure ulcers is essential to reduce their economic and human impact on patients and the healthcare system.
To prevent these ulcers, we should know the risk factors which are partly "mechanical" and partly "medical". The following are the major ones and notice how these factors can overlap.
Risk Factors
Heel Pressure Ulcers typically follow a chain of events
1. Immobility: Patients who are bedridden, wheelchair-bound, or have limited mobility are at a higher risk of developing pressure ulcers.
Immobility is one of the foremost risk factors contributing to the development of heel pressure ulcers. Patients who cannot change position independently due to conditions such as stroke, neurological disorders, or advanced age often experience prolonged pressure on specific areas of the body, particularly the heels, sacrum, elbows and other points of bony prominence.
The lack of movement reduces blood flow to the skin, as the pressure applied to the tissue, even when slight, is unremitting. This situation increases the likelihood of tissue damage and pressure ulcer formation. The mechanics of the situation can be complex and the only safe level of pressure is Zero.
Heel ulcer mechanical scenario
In acute care settings, it's crucial to implement strategies that encourage regular repositioning of immobile patients. This can be achieved when feasible through scheduled turning, pressure-relieving devices, and engaging patients in passive range-of-motion exercises.
The urgency of addressing immobility cannot be overstated. Early intervention can significantly reduce the risk of ulcer development, ultimately leading to better patient outcomes and lower healthcare costs. Continuous assessment and personalised care plans are vital for identifying at-risk patients and effectively implementing preventative measures.
2. Age: Older adults have thinner, more fragile skin and are more susceptible to skin damage.
The impact of age as a risk factor for heel pressure ulcers is particularly concerning, given the demographic shift towards an ageing population in many countries, including the UK. As individuals age, physiological changes such as decreased collagen production and reduced elasticity impact skin integrity, making it more prone to breakdown under pressure and shear forces. Additionally, older adults may experience comorbid conditions such as diabetes, vascular diseases, or malnutrition, which further compromise skin health and healing capabilities.
It is imperative for healthcare professionals to implement targeted assessments and interventions for older patients, focusing on skin inspections, education about skincare routines, and the use of protective barriers. With the increasing prevalence of age-related factors in healthcare settings, an urgent need emerges to develop comprehensive training and protocols that address the unique vulnerabilities of elderly patients. Proactive measures can mitigate risks and significantly enhance overall patient care, reducing the human suffering associated with pressure ulcers and the economic burden on the healthcare system. It's also important to remember that prolonged bed rest is particularly damaging for the elderly, resulting in a heightened risk of pressure ulcers and muscle weakness that may extend hospital stays and permanently reduce a return to independence.
3. Poor nutrition: Malnutrition and dehydration can reduce the skin’s ability to withstand pressure and heal wounds.
Poor nutrition poses a significant risk for developing heel pressure ulcers, as malnutrition and dehydration substantially impair skin integrity and the body's ability to heal. Insufficient intake of essential nutrients, such as proteins, vitamins, and minerals, can weaken the skin's structural components, making it more susceptible to damage from sustained pressure. For instance, protein is crucial for maintaining skin elasticity and promoting wound healing, while vitamins C and E play vital roles in collagen synthesis and antioxidant protection.
Furthermore, hydration is equally important; a lack of adequate fluid intake can lead to dry, brittle skin that is more prone to injury. In clinical settings, addressing nutritional deficiencies should be a priority, particularly for patients with existing risk factors or those recovering from illness or surgery. Regular nutritional assessments and interventions tailored to individual dietary needs can significantly reduce the risk of pressure ulcers. The urgency for healthcare providers to proactively address poor nutrition cannot be overstated, as timely and appropriate nutritional support can enhance overall patient outcomes, reduce complications, and alleviate the financial strain on healthcare systems associated with treating pressure ulcers. Encouraging a multidisciplinary approach, including collaboration with dietitians, can further ensure that patients receive the comprehensive care necessary to prevent these serious complications.
4. Incontinence: Patients with urinary or faecal incontinence are at a higher risk of developing pressure ulcers due to prolonged skin exposure to moisture.
Incontinence is a critical risk factor for developing heel pressure ulcers, as it often results in prolonged skin exposure to moisture, compromising its integrity. The presence of urine or faeces can lead to skin maceration, making it more susceptible to pressure injuries. This situation is particularly concerning for patients who cannot clean themselves adequately or have caregivers who may overlook the importance of timely hygiene interventions. The urgency to address incontinence must be a priority in care plans; utilising appropriate absorbent products, implementing scheduled toileting regimens, and maintaining skin care protocols are essential strategies to mitigate this risk. Additionally, healthcare professionals must foster open communication with patients and their families regarding the importance of managing incontinence effectively. Doing so can help prevent the onset of pressure ulcers, enhance the overall quality of care, and reduce the associated healthcare costs.
5. Chronic diseases: Patients with chronic conditions such as diabetes, cardiovascular disease, or neurological disorders are at a higher risk of developing pressure ulcers due to impaired circulation and sensation.
Chronic conditions, particularly diabetes, significantly elevate the risk of developing pressure ulcers due to their detrimental effects on tissue viability, peripheral circulation and sensation. Individuals with diabetes often experience peripheral neuropathy, which can progressively impair their ability to feel pressure or pain, consequently failing to recognise when they are at risk for developing pressure injuries.
Additionally, diabetes can lead to vascular complications that hinder blood flow to the skin, compromising its ability to withstand pressure and heal effectively. The combination of decreased sensation and poor circulation creates a precarious situation, making it essential for healthcare providers to implement consistent monitoring and tailored care plans for diabetic patients. Urgency is paramount; by actively managing diabetes and its complications, healthcare professionals can mitigate the risk of pressure ulcers, improve patient outcomes, and reduce the financial burden on healthcare systems.
6. Poor personal hygiene can increase the risk of developing pressure ulcers.
Poor hygiene represents a significant risk factor for developing pressure ulcers, particularly among vulnerable patient populations. Inadequate personal cleanliness can accumulate bacteria and moisture on the skin, severely compromising skin integrity and increasing susceptibility to injury. The presence of dirt, sweat, and other bodily fluids can exacerbate skin breakdown, especially in regions where pressure is concentrated. It is essential for healthcare professionals to prioritise diligent hygiene practices as part of comprehensive patient care. This includes regular bathing, the use of appropriate skin cleansers, and consistent monitoring of skin condition. The urgency of addressing poor hygiene cannot be overstated, as proactive measures protect the skin from damage, enhance healing, and ultimately reduce the incidence of pressure ulcers, thereby improving patient quality of life and mitigating potential healthcare costs associated with treatment complications.
7. Smoking: Smoking reduces blood flow to the skin, making it more susceptible to pressure ulcers.
Smoking is a critical risk factor for the development of pressure ulcers, as it significantly reduces blood flow to the skin. This compromised circulation diminishes the delivery of essential nutrients and oxygen necessary for maintaining healthy skin and effective wound healing. Additionally, the harmful substances in tobacco can impair the body's inflammatory response, further complicating the healing process. For patients at higher risk of pressure ulcers, such as those with existing health conditions or limited mobility, it is imperative to address smoking cessation as a fundamental component of their care. The urgency to implement smoking cessation strategies cannot be overstated; by reducing smoking rates among these patients, healthcare providers can markedly enhance skin integrity, promote healing, and ultimately lower the incidence of pressure ulcers, contributing to improved overall patient outcomes and reduced healthcare costs.
8. Cognitive impairment: Patients with cognitive impairment may be less likely to recognize discomfort or take action to alleviate pressure.
Cognitive impairment presents a significant challenge in the prevention of pressure ulcers, as individuals affected by conditions such as dementia or other neurological disorders may struggle to identify discomfort or respond appropriately to physical cues. This inability to communicate pain or to understand the necessity of repositioning can lead to prolonged periods of pressure on vulnerable areas of the skin, drastically increasing the risk of ulceration. The urgency to adequately assess and support these individuals is paramount; healthcare providers must implement tailored care strategies, including regular skin assessments and frequent repositioning schedules. Engaging caregivers and family members in the care process is critical, as well as ensuring they are educated about the signs of discomfort and the importance of proactive intervention. By prioritising the needs of patients with cognitive impairment, healthcare professionals can significantly reduce the incidence of pressure ulcers, enhance overall patient care, and alleviate potential burdens on healthcare resources.
9. Poor positioning: Patients positioned improperly or who spend too much time in one position are at a higher risk of developing pressure ulcers.
Poor positioning plays a critical role in developing heel pressure ulcers, as it can lead to sustained pressure and unrelieved strain on the delicate skin and underlying tissues of the heel. When patients remain in one position for extended periods, particularly those immobile or have limited ability to shift their weight, the constant pressure can impede blood flow and compromise tissue oxygenation. This scenario is particularly concerning for patients with conditions that already affect circulation, as the heels are specifically vulnerable due to their anatomical structure and exposure to external forces.
The consequence of neglecting appropriate positioning strategies not only heightens the likelihood of heel pressure ulcers but can also result in pain, infection, and extended hospital stays, ultimately complicating patient recovery. Given these significant risks, it is imperative for healthcare providers to regularly assess positioning techniques and implement preventive measures to mitigate heel pressure ulcer development, thereby safeguarding patient health and reducing healthcare costs associated with treatment and recovery.
10. Medical devices: Patients who use medical devices such as catheters or oxygen masks may be at a higher risk of developing pressure ulcers in the areas where the device contacts the skin.
It’s important to note that the relative importance of these risk factors can vary depending on the patient’s individual circumstances. Healthcare professionals should conduct a comprehensive assessment to identify patients at risk of developing pressure ulcers.
What the PRAFO range offers
The PRAFO (Pressure Relief Ankle Foot Orthosis) range presents a valuable orthotic management solution in the context of pressure ulcer prevention and management, particularly concerning heel pressure ulcers. These orthoses are specifically designed to relieve pressure from vulnerable heel areas, reducing the risk of skin breakdown in compromised patients. In fact the PRAFO range are designed to completely eliminate pressure at the heels and prevent other complications such as the development of foot and ankle contractures.
The structure of the PRAFO range products uniquely allow adjustment and protected ambulation
By facilitating better positioning and enhancing blood circulation, the PRAFO range addresses several critical risk factors associated with heel ulcers, such as immobility and improper positioning. Furthermore, the implementation of PRAFO devices can significantly aid in the holistic management plan for at-risk patients, particularly those with cognitive impairments or other health complications.
An important and sometimes overlooked issue is continuity of care. The PRAFO range facilitates protect whether the patient is in bed or when ambulant. This is important as it minimises bed rest which is so important to achieving a good clinical outcome.
Conclusion
Given the alarming incidence rates of pressure ulcers and the resultant impact on patient health and healthcare costs, incorporating the PRAFO range into patient care protocols provides an urgent and effective strategy. By prioritising the use of dedicated orthotic devices like PRAFO, healthcare professionals can better safeguard skin integrity, improve patient comfort, and ultimately enhance recovery outcomes, reinforcing the importance of a proactive approach to pressure ulcer prevention and treatment.
Related Articles
How to Choose the Best Heel Protectors for Pressure Ulcer Prevention or Treatment
How to Prevent Heel Pressure Ulcers: First Understand What Causes Them?