Heel Ulcers: Symptoms, Causes, and Treatments
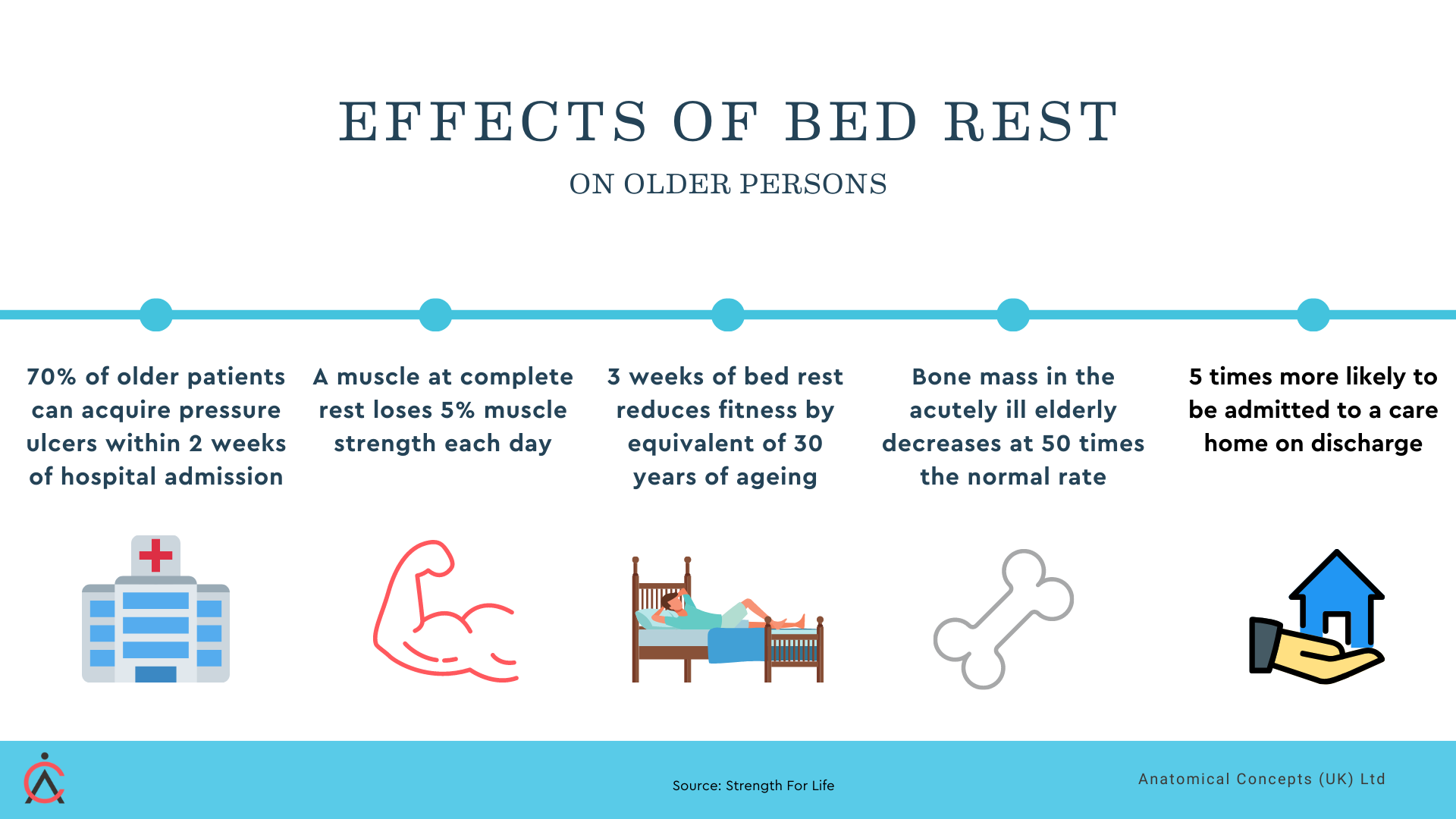
A heel ulcer, also known as a pressure ulcer or, in the past, as a pressure sore, is a wound that develops from prolonged pressure on the skin and underlying tissue. It is most common in the elderly who may be immobile and nutritionally challenged - and those with medical conditions such as diabetes, peripheral arterial disease, or spinal cord injury. Heel ulcers occur when pressure is applied to the heel for extended periods, cutting off blood flow to the localised tissue and causing skin and subcutaneous tissue damage.
Heel ulcers are not a new problem. They represent a massive cost to the NHS and of course an emotional and physical burden on those who experience them. In this article we describe the characteristics of heel ulcers and the role of the PRAFO range in their prevention or treatment.
Symptoms of Heel Ulcers
Early signs of developing heel ulcers include redness, warmth, or a blister-like area on the skin. As the ulcer progresses, the skin may appear discoloured, blackened, or have a scab-like appearance. The wound may have a foul odor and may produce drainage if infected. If left untreated, heel ulcers can extend into deeper tissue, leading to tissue loss, nerve damage, and disfigurement
Causes of Heel Ulcers
Heel ulcers develop when there is excessive pressure on an area of skin overlying a bony prominence for an extended period of time. The challenge is made more difficult because what is “excessive” pressure and “extended” time is highly variable. In fact it is safest to say that there is no absolutely safe level of pressure.
This pressure can be caused by lying or sitting in the same position for too long, especially when there is decreased mobility, such as in the elderly or those in intensive care or with paralysis due to spinal cord injury. When the skin and subcutaneous tissue are compressed because of contact with a support surface, blood flow is restricted, and tissue damage occurs of the situation persists for long enough. Other factors that can contribute to the development of heel ulcers include:
Vascular disease that impairs blood flow to the skin and local tissue
Peripheral neuropathy, (often associated with a diabetic foot ulcer) which affects the nerves that sense pain and pressure
Diabetes, which can lead to decreased blood flow to the feet and a weakened immune system
Incontinence or skin moisture, which can weaken the skin's integrity and lead to skin breakdown
Poor manual handling techniques - for example moving a person on a support surface resulting in friction and shear bettween the heel and the support surface.
Treatment of Heel Ulcers
We should say at once that the best approach is always prevention. Every patient at risk should use a PRAFO on each foot. But - if the worst should happen…
Treatment of heel ulcers involves wound care to promote healing and prevent infection. This can include the podiatrist removing dead tissue or eschar, applying dressings to promote wound healing, and providing pressure relief to the affected area.
Whatever else is done - pressure relief is paramount.
Depending on the severity of the ulcer, a healthcare professional may recommend the use of medical devices like heel protectors or pressure relief cushions to reduce pressure on the wound. It is essential to keep the wound clean and dry, avoid putting weight on the affected heel, and maintain good nutrition to promote wound healing.
The PRAFO range of heel pressure relief products are the market leading devices for heel pressure relief as they don't just reduce heel pressure - they totally eliminate it.
Cushions and other devices that still contact the heel may seem attractive due to their lower cost but will still allow the consequences of prolonged pressure and time to cause problems.
Continuity of care is also an important reason for choosing from the PRAFO range.
Continuity of care refers to the consistent and coordinated provision of care to an individual patient over time, with a focus on maintaining their wellbeing and preventing further health issues. All too often we see short term “fire fighting” - confronting the current problem without thinking about what comes next.
Continuity of care involves good communication and collaboration between healthcare providers across different settings (e.g. hospitals, clinics, long-term care facilities) to ensure that the patient's needs are met and that their care is streamlined and efficient over time.
When it comes to managing heel ulcers, continuity of care can play a crucial role in promoting healing and preventing further damage. This is where PRAFO (Pressure Relief Ankle Foot Orthosis) can come into play.
These devices are designed to provide foot and ankle support while also relieving pressure on the heel, which can be especially helpful for individuals with heel ulcers who may be at risk of developing plantarflexion deformities (such as those recovering from stroke).
By thinking about continuity of care we might, for example, recognise that a patient currently in bed and needing heel protection, will shortly need to be mobilised and then walking in a community setting. The PRAFO range has features that prevent or treat heel ulcers, maintain foot and ankle alignment and then allow safe mobilisation - all with one product. Try doing that with "pressure relief cushion".
If we take the example of an older person, it can be particularly important to avoid prolonged bed rest. By using a suitable PRAFO the patient can be protected in bed and the same device used to mobilise the patient at the earliest opportunity.
Prevention of Heel Ulcers
As stated above, preventing heel ulcers is key to avoiding the pain and discomfort associated with these wounds. Simple steps to prevent heel ulcers include regular repositioning, reducing pressure on bony areas by using pressure relief devices (ideally the PRAFO), good skin care, and managing medical conditions that can contribute to ulcer development. Regular foot checks can also help identify early signs of infection or skin breakdown that can lead to ulcers.
Early intervention is crucial for preventing complications associated with pressure ulcers, such as infection, tissue loss, or nerve damage. If a patient does develop a pressure ulcer, healthcare professionals should provide prompt intervention to promote wound healing, prevent infection, and manage pain. This may involve referral to a wound care specialist or other healthcare professional with expertise in pressure ulcer management and wound care.
Conclusion
Heel ulcers are a common problem for patients with decreased mobility or underlying medical conditions, such as diabetes or vascular disease. Understanding the causes and symptoms of heel ulcers is key to preventing these wounds from developing and promoting overall skin health. Healthcare professionals play an important role in preventing and managing pressure ulcers and should be familiar with the latest evidence-based practices for pressure ulcer prevention and management. By implementing preventive measures, providing education, and providing prompt intervention, healthcare professionals can help reduce the burden of pressure ulcers for patients and improve their quality of life.
All patient’s at risk should in our view be provided with appropriate heel protection and the PRAFO range represents the leading device of it’s type. If you need guidance on any of the range please ask.