A Comprehensive Guide to Lower Motor Neuron Lesions: Causes, Symptoms, Diagnosis, and Treatment Options
Delving into the complex world of lower motor neuron lesions and their impact on daily life
Introduction
Lower motor neuron lesions can have a profound effect on the nerves responsible for controlling movement in the body, leading to a range of symptoms, including muscle weakness and atrophy (loss of muscle bulk). These conditions can be caused by various factors, such as injury, disease, and even genetic disorders.
In our work we mostly meet individuals who have experienced a spinal cord injury that has resulted in damage to the Lower Motor Neurons resulting in denervation of muscle. We also see nerve injuries such as a Brachial Plexus injury to the shoulder.
In this guide, we will explore some of the causes, the symptoms, diagnosis, and treatment options for lower motor neuron lesions, highlighting the importance of early intervention and appropriate care.
Understanding Lower Motor Neuron Lesions
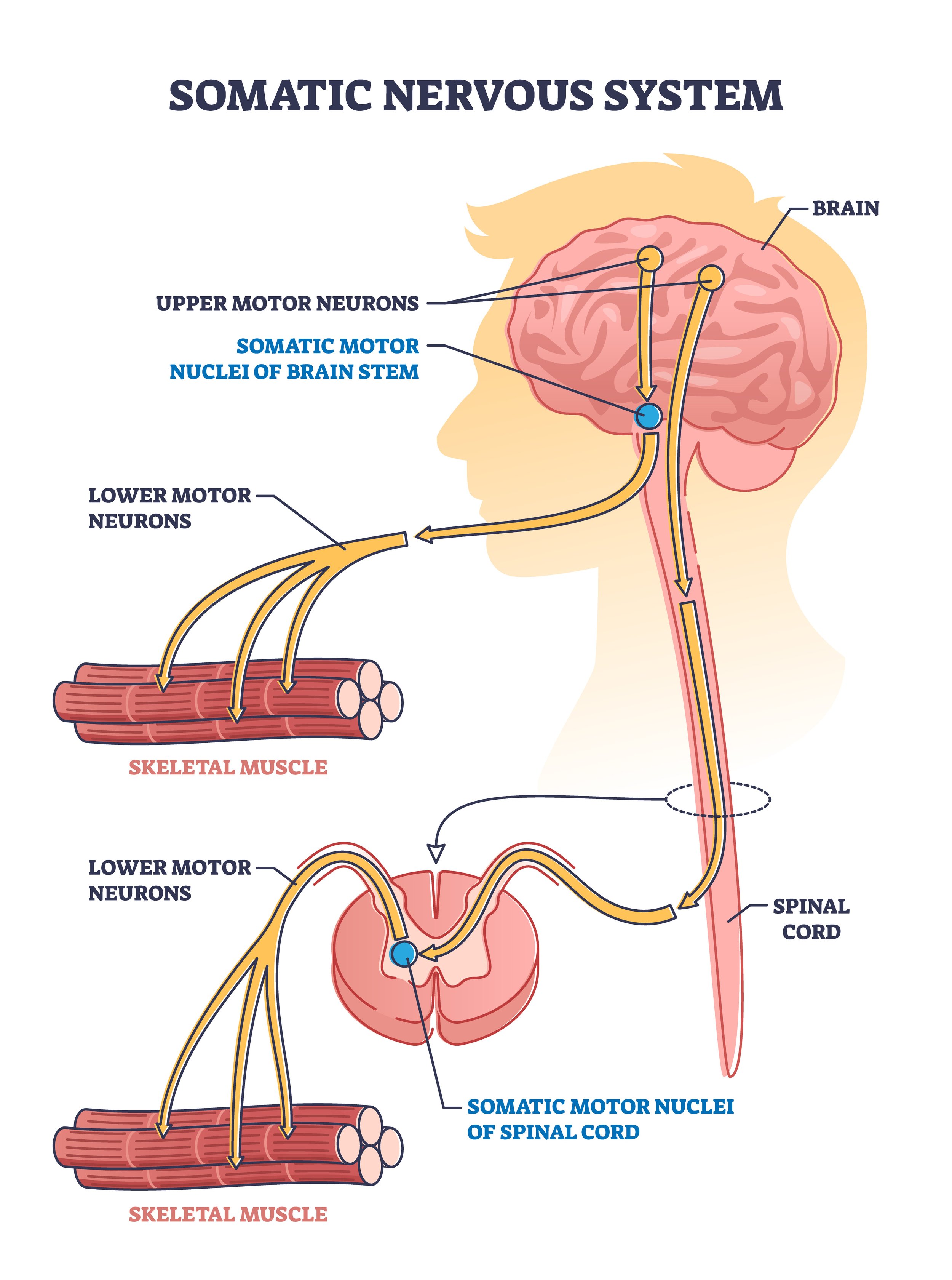
Lower motor neuron lesions involve damage or dysfunction of the nerves that connect the spinal cord to the muscles in the body. See adjacent figure.
These nerves play a crucial role in controlling voluntary movements, such as walking, reaching, and grasping. Damage to these nerves can lead to muscle weakness, atrophy, and other symptoms such as fasciculations (see below), and loss of reflexes. This will significantly impact a person's ability to move and perform daily activities.
We know that over time, the structure of affected muscles and nerves will change due to this denervation.
As the muscle typically becomes smaller it also loses it’s essential structure and basically muscle fibres are gradually replaced with tissue that is not able to contract - tissue formed of fat and collagen. This represents a problem because it reflects the development of poor tissue health and hence vunerability to serious issues such as compromised circulation and pressure ulcers.
At Anatomical Concepts we are often seeing clients with denervation of particular muscle groups due to spinal cord injury.
Lower motor neurons (LMNs) are found throughout the entire length of the spinal cord, with their cell bodies located in the anterior (ventral) horn of the gray matter. Damage to LMNs can occur at any spinal cord injury level, but the specific consequences will depend on the location of the injury.
Cervical spinal cord injuries (C1-C8) can affect the LMNs that control the muscles of the arms, hands, and diaphragm. Damage at this level may result in denervation of the upper extremities and potentially cause breathing difficulties.
Thoracic spinal cord injuries (T1-T12) can affect the LMNs that control the muscles of the trunk and some parts of the upper extremities. Damage at this level may result in denervation of the trunk muscles, leading to difficulties with trunk stability, balance, and posture.
Lumbar spinal cord injuries (L1-L5) can affect the LMNs that control the muscles of the lower extremities, including the hips, thighs, and lower legs. Damage at this level may result in denervation of the lower extremities, leading to difficulties with mobility, such as walking and standing.
Sacral spinal cord injuries (S1-S5) can affect the LMNs that control the muscles of the pelvic region, as well as bowel and bladder function. Damage at this level may result in denervation of the pelvic muscles, leading to difficulties with bowel and bladder control and sexual function.
It is important to note that the severity of denervation and the extent of functional loss depend on the degree of damage to the LMNs. In some cases, partial damage may result in only mild symptoms, while more extensive damage can lead to complete loss of function in the affected areas.
Identifying the Causes of Lower Motor Neuron Lesions
Lower motor neuron lesions and the resulting denervation can be attributed to a diverse range of factors, such as:
Physical injuries - trauma affecting the nerves
Viral or bacterial infections
Autoimmune disorders
Genetic disorders
Certain medications
In some instances, the cause may remain unknown. Collaborating with a healthcare professional to pinpoint the underlying cause of the lesion is crucial for developing an appropriate treatment plan.
Recognising the Symptoms of Lower Motor Neuron Lesions
The symptoms associated with lower motor neuron lesions can vary, depending on the location and severity of the damage. Common symptoms include:
Muscle weakness
Muscle atrophy (shrinkage)
Muscle twitching
Difficulty with movement and coordination
Muscle cramps
Fasciculations (involuntary muscle contractions)
Muscle stiffness
Promptly seeking medical attention upon experiencing these symptoms is vital, as early diagnosis and treatment can significantly improve outcomes.
Diagnosis of Lower Motor Neuron Lesions
Diagnosing lower motor neuron lesions typically involves a combination of physical examination, medical history, and diagnostic tests. A clinician may:
Perform a neurological exam to assess muscle strength, reflexes, and coordination
Order imaging tests such as MRI or CT scans to visualize the affected area
Conduct electrophysiological studies, including electromyography (EMG) and nerve conduction studies, to evaluate nerve and muscle function
A thorough evaluation is essential for an accurate diagnosis. Sometimes we meet individuals who only recognise that they have an issue when they try an FES Cycling system such as the RehaMove. They discover that no mucle contractions are produced as a result of the neuromuscular electrical stimulation that is inherent to these systems; because these units rely on having intact lower motor neurons to work.
Treatment Options for Lower Motor Neuron Lesions
Treatment for lower motor neuron lesions depends on the underlying cause and severity of the condition. Possible treatment options include:
Time and rest, allowing the lesion to heal on its own in some cases
Physical therapy and occupational therapy to improve muscle strength and function
Medications, such as muscle relaxants and pain relievers, to manage symptoms
Surgery to repair or remove the affected nerve or muscle in more severe cases
Electrotherapy which has been shown by research to restore the bulk and tissue quality. In cases where re-innervation is expected or surgery is intended, then electrotherapy can preserve the structure of the tissue to take advantage of this opportunity.
The Stimulette RISE
Although electrotherapy for treatment of lower motor neurons was once controversial, there is now a great deal of evidence supporting it’s effectiveness with complete and incomplete lesions. Electrotherapy in these cases typically uses a prinicple in which muscle fibres are directly stimulated rather than relying on the nerve structure - which is of course damaged.
Anatomical Concepts has many users working with the RISE unit at home and the main challenge is that to be effective at restoring tissue quality and bulk of the muscles it needs to be used at least 5 days per week for around 30 minutes per muscle group.
Collaborating closely with a healthcare provider is crucial in determining the most appropriate course of treatment for each individual's unique needs.
Conclusion
Lower motor neuron lesions can have a significant impact on an individual's ability to move and perform daily activities. Early diagnosis and appropriate treatment are essential for achieving the best possible outcomes. By understanding the causes, symptoms, diagnosis, and treatment options for lower motor neuron lesions, individuals affected can be supported.
We have written a number of articles exploring the application of the Stimulator RISE and links to these articles can be found below.
https://www.anatomicalconcepts.com/articles/evaluating-denervated-muscle-with-the-rise-stimulator
https://www.anatomicalconcepts.com/articles/why-you-should-treat-denervated-muscle-quickly
https://www.anatomicalconcepts.com/articles/what-can-i-do-to-help-denervated-muscles
https://www.anatomicalconcepts.com/articles/can-you-stimulate-a-denervated-muscle